Abstract
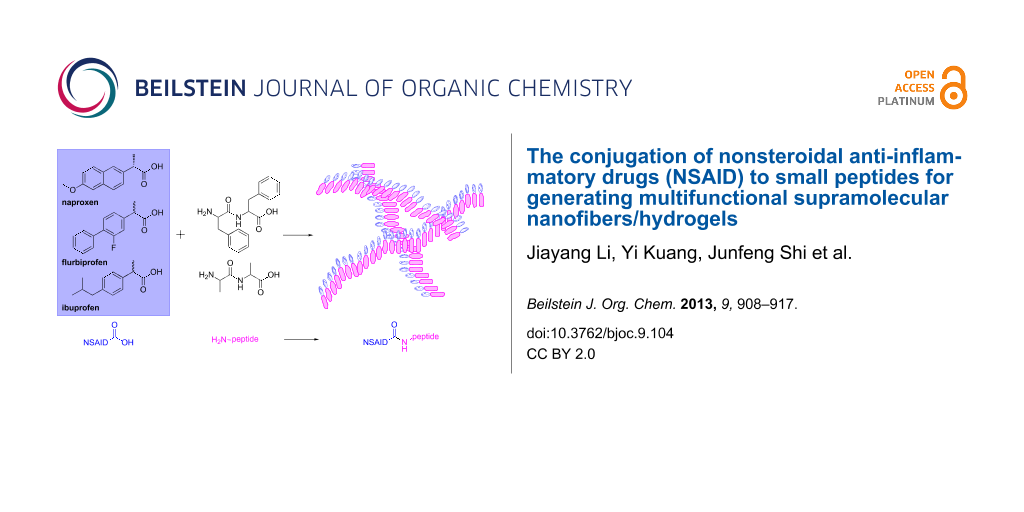
Here we report supramolecular hydrogelators made of nonsteroidal anti-inflammatory drugs (NSAID) and small peptides. The covalent linkage of Phe–Phe and NSAIDs results in conjugates that self-assemble in water to form molecular nanofibers as the matrices of hydrogels. When the NSAID is naproxen (1), the resultant hydrogelator 1a forms a hydrogel at a critical concentration (cgc) of 0.2 wt % at pH 7.0. Hydrogelator 1a, also acting as a general motif, enables enzymatic hydrogelation in which the precursor turns into a hydrogelator upon hydrolysis catalyzed by a phosphatase at physiological conditions. The conjugates of Phe–Phe with other NSAIDs, such as (R)-flurbiprofen (2), racemic flurbiprofen (3), and racemic ibuprofen (4), are able to form molecular hydrogels, except in the case of aspirin (5). After the conjugation with the small peptides, NSAIDs exhibit improved selectivity to their targets. In addition, the peptides made of D-amino acids help preserve the activities of NSAIDs. Besides demonstrating that common NSAIDs are excellent candidates to promote aromatic–aromatic interaction in water to form hydrogels, this work contributes to the development of functional molecules that have dual or multiple roles and ultimately may lead to new molecular hydrogels of therapeutic agents for topical use.
Graphical Abstract
Introduction
This article reports the design, synthesis, and characterization of hydrogelators made of non-steroidal anti-inflammatory drugs (NSAID) and small peptides for the development of multifunctional supramolecular hydrogels. Sharing similar features with the extracellular matrices of tissues (e.g., consisting of three-dimensional networks and a significant amount of water), hydrogels have become an attractive choice for developing biomaterials for a variety of applications. For example, hydrogels have frequently served as scaffolds for tissue engineering and as carriers for drug delivery [1-4]. In the applications of drug delivery, it is common to use hydrogels made of biodegradable polymers to encapsulate therapeutic agents for controlled release of drugs by adjusting the pore sizes and functionality of the polymer networks [5,6]. Despite the tremendous success of this approach, several inherent shortcomings still limit the application of polymeric hydrogels. For example, the degradation of the polymers usually generates acidic monomers, which, sometimes, cause undesired inflammatory responses [7]. In most of the cases, the polymers themselves are passive, which unavoidably results in the limited loading of drug molecules [8,9]. Though possible, it is relatively difficult to functionalize the polymers with drug molecules. Even though it has been attempted, the release of the drugs from the polymer backbone remains a nontrivial issue. Despite being constantly improved, these limitations call for the exploration and development of new functional biomaterials and therapeutics.
The recent development of supramolecular nanofibers and hydrogels [10-25] presents an exciting opportunity for developing new types of biomaterials [26-29]. While the early works have centered on the use of nanofibers of oligopeptides to form hydrogels as a passive scaffold for tissue engineering and drug delivery [30], the seminal work by Stupp et al., in which functional hydrogels based on supramolecular nanofibers regulate the differentiation of neural progenitor cells [31], has demonstrated undoubtedly the power and promises of the rational incorporation of functional motifs into the building blocks of the supramolecular nanofibers and hydrogels. Besides being used for three-dimensional cell cultures [32], supramolecular hydrogels also find applications in typing [33] and against bacteria [34-38], and in enzyme assays [23,39], catalysis [40], and inhibiting cancer cells [41-44]. These successful examples further underscore the potentials of functional supramolecular hydrogels as new and useful biomaterials.
Since the formation of supramolecular hydrogels relies on the small molecules (i.e., the hydrogelators) that self-assemble in water through noncovalent interactions [45,46], these hydrogels are inherently easily biodegradable. To meet the prerequisites for self-delivery systems, besides biodegradability, the hydrogelators should preserve the pharmacological efficacy of the therapeutic building blocks, any side effects should be minimized and the biocompatibility maximized. Therefore, a convenient starting point for developing the molecular hydrogels of therapeutic agents is to construct hydrogelators only consisting of the therapeutic agent and biocompatible motifs [47,48]. Among a large pool of therapeutic agents, we choose to develop the molecular hydrogels of NSAIDs because topical use of the hydrogels of NSAIDs is an attractive therapeutic option for treating acute pain [49].
Because of their analgesic, antipyretic, and anti-inflammatory effects (when being used in high dosage), NSAIDs are widely used for the treatment of acute or chronic pain or inflammations. Despite the widespread systemic use of NSAIDs, the adverse gastrointestinal and renal effects and cardiovascular risks associated with NSAIDs have led to the development of topical NSAIDs formulations, such as patch, gel, and solution [50-52]. Encouraged by the successful FDA approval of diclofenac gel [53] and several reports of small molecule hydrogels formed by NSAID derivatives [48,54-56] we intend to explore supramolecular hydrogels of other NSAIDs. Specifically, we use naproxen (denoted as Npx in this report), an over-the-counter NSAID, to generate a new hydrogelator 1a that only consists of naproxen and diphenylalanine (FF). We use diphenylalanine because it is able to self-assemble to form nanotubes [57]. We find that compound 1a, forming a hydrogel at the critical gelation concentration (cgc) of 0.2 wt % at pH 7.0, also serves as a general motif to enable enzymatic hydrogelation that converts 1c to 1d by a phosphatase and results in a hydrogel of 1d under physiological conditions. In addition to naproxen, we evaluate the abilities of other NSAIDs (Scheme 1) as building blocks of hydrogelators and find that the conjugates of FF and (R)-flurbiprofen (2), racemic flurbiprofen (3) or racemic ibuprofen (4) form supramolecular hydrogels. Moreover, our previous examination of the efficacy of the hydrogelators derived from naproxen shows that the conjugation of small peptides may improve the selectivity of naproxen for inhibiting COX-2 and thus reduces their adverse effect [58]. Although the inhibition efficacies of the hydrogelators for both enzymes COX-1 and COX-2 are lower than naproxen, the use of D-peptide for conjugation helps preserve the activities of naproxen. These results provide useful insights for the optimization of these hydrogelators. Besides serving as a potential alternative approach to polymeric hydrogels [59,60], this work contributes to the development of bioactive molecules that have dual or multiple roles, for example, as therapeutic agents and delivery carriers [61,62].
Scheme 1: The structures of the NSAIDs and peptides explored as the building blocks of hydrogelators in this work.
Scheme 1: The structures of the NSAIDs and peptides explored as the building blocks of hydrogelators in this ...
Results and Discussion
Synthesis
Scheme 2 shows the typical synthetic route of the conjugates of NSAID and small peptides exemplified in the case of naproxen. In this process, naproxen (1) first reacts with N-hydroxysuccinimide (NHS) and N,N'-dicyclohexylcarbodiimide (DCC) in chloroform to afford the NHS ester of 1, which reacts with a phenylalanine in the mixed solvent of acetone and water to produce 11. The same coupling procedure allows the covalent attachment of second phenylalanine on the C-terminal of 11 to give 1a. Being activated by NHS, 1a reacts with phosphotyrosine (pY) to yield 1c after purification by HPLC. Using the same procedure, we connect naproxen to D-peptides to make Npxff (1b), Npxffy(p) (1e), and Npxffy (1f), because D-amino acid based hydrogelators are able to resist proteases [63].
Scheme 2: The synthetic route of the naproxen-containing hydrogelators and the corresponding precursors: (i) NHS, DCC, CHCl3, 2 h; Phe, pH 8.5, 12 h. (ii) NHS, DCC, CHCl3, 12 h; Tyr(p), pH 8.5, 24 h. (iii) alkaline phosphatase, pH 7.6.
Scheme 2: The synthetic route of the naproxen-containing hydrogelators and the corresponding precursors: (i) ...
Scheme 2 shows the general synthetic route of other NSAID containing hydrogelators and lists all the NSAID-based conjugates studied in this work. Generally, after reacting with NHS and DCC in chloroform, the NSAID becomes a NHS ester, which reacts with the small peptides (e.g., Phe–Phe, Phe–Phe–Tyr, or Ala–Ala) in the mixed solvent of acetone and water. We have produced these NSAID-containing hydrogelators with yields from 40% to 60% after purification by HPLC or column chromatography. For example, flurbiprofen (R-enantiomer 2 or racemic 3) conjugates with L- or D-diphenylalanine to afford compounds (R)-Fbp-FF (2a), (R)-Fbp-ff (2b), and (RS)-Fbp-FF (3a) (Fbp = flurbiprofen). The attachment of racemic ibuprofen to L-diphenylalanine yields compound (RS)-Ibp-FF (4a) (Ibp = ibuprofen). Since the direct use of acetylsalicylic acid (aspirin) to connect with dipeptides results in a compound hydrolyzing easily at the ester bond of aspirin, we use salicylic acid (Sal) instead to conjugate with diphenylalanine and dialanine (AA) to make compounds 5a and 5g, respectively.
Self-assembly and hydrogelation
After the synthesis of the NSAID/small-peptid conjugates, we examined the capability of the conjugates to self-assemble in water to form supramolecular nanofibers and hydrogels (Table 1). Typically, the addition of 8.0 mg of Npx-FF (1a) into 1.0 mL of water under basic conditions (pH 9.0) affords a solution, which turns into a suspension at pH 7.0. Upon heating to 60 °C, the suspension turns to a clear solution, and then becomes a transparent hydrogel after being cooled to room temperature (Figure 1A). The treatment with a small amount of base prior to the adjustment of pH appeared to be a necessary step for making the hydrogel. Being thermally reversible and relatively sensitive to the temperature, the hydrogel of 1a exhibits excellent recovery properties (Supporting Information File 1, Figure S4) [64].
Table 1: The properties of the NSAID-containing hydrogels.
|
concentration
(wt %) |
pH | method of preparation | components | gel properties | |
|---|---|---|---|---|---|
| 1a | 0.8 | 7.0 | heat–cool | naproxen, L-Phe–L-Phe | transparent gel, thermal reversible, mechanical recovery |
| 1b | 0.8 | 4.0 | acidic pH | naproxen, D-Phe–D-Phe | opaque hydrogel, precipitate at high T, |
| 1d | 1.5 | 7.6 | enzyme | naproxen, L-Phe–L-Phe–L-Tyr | transparent gel, mechanical recovery |
| 1f | 0.8 | 7.6 | enzyme | naproxen, D-Phe–D-Phe–D-Tyr | transparent gel |
| 2a | 0.8 | 7.2 | heat–cool | (R)-flurbiprofen, L-Phe–L-Phe | slightly opaque hydrogel, thermal reversible, weak mechanical recovery |
| 2b | 0.8 | 7.2 | heat–cool | (R)-flurbiprofen, D-Phe–D-Phe | semitransparent hydrogel, thermal reversible, weak mechanical recovery |
| 3a | 0.8 | 7.2 | heat–cool | (RS)-flurbiprofen, L-Phe–L-Phe | semitransparent hydrogel, thermal reversible, weak mechanical recovery |
| 4a | 0.8 | 7.2 | heat–cool | (RS)-ibuprofen, L-Phe–L-Phe | semitransparent hydrogel, thermal reversible, weak mechanical recovery |
| 1g | 0.8 | 4.0 | acidic pH | naproxen, L-Ala–L-Ala | opaque hydrogel, poor stability at rt |
| 3g | 0.8 | 1.0 | acidic pH | (RS)-flurbiprofen, L-Ala–L-Ala | opaque hydrogel, poor stability at rt |
![[1860-5397-9-104-1]](/bjoc/content/figures/1860-5397-9-104-1.jpg?scale=3.2&max-width=1024&background=FFFFFF)
Figure 1: Optical images of the hydrogels formed by (A) 1a (0.8 wt %, pH 7.0); (B) 1b (0.8 wt %, pH 4.0); (C) 1d (1.5 wt %, pH 7.6), obtained by treating 1c with alkaline phosphatase (5.0 U/mL); (D) 1f (0.8 wt %, pH 7.6), obtained by treating 1e with alkaline phosphatase (5.0 U/mL); (E) 2a (0.8 wt %, pH 7.2); (F) 2b (0.8 wt %, pH 7.2); (G) 3a (0.8 wt %, pH 7.2); (H) 4a (0.8 wt %, pH 7.2); (I) 1g (0.8 wt %, pH 4.0); (J) 3g (0.8 wt %, pH 1.0).
Figure 1: Optical images of the hydrogels formed by (A) 1a (0.8 wt %, pH 7.0); (B) 1b (0.8 wt %, pH 4.0); (C) ...
The hydrogelation of 1a also offers an opportunity to examine whether the attachment of a tyrosine phosphate residue to 1a allows enzymatic hydrogelation. As a soluble precursor, 1c (15.0 mg) dissolves in water (1.0 mL) at pH 7.6. After being treated with alkaline phosphatase (5.0 U/mL), the solution of 1c quickly transforms to a clear hydrogel within one hour. Due to the additional tyrosine residue, 1d, however, exhibits much better solubility in water than does 1a. Thus, 1d remains as a solution at the concentration of 0.8 wt %, and only forms a stable hydrogel (Figure 1C) when the concentration of 1d reaches 1.5 wt %. As in the case of 1a, the hydrogel of 1d also shows good recovery properties.
Being the diastereomer of 1a, hydrogelator 1b exhibits quite different behavior in terms of self-assembly and hydrogelation. For example, at a concentration of 0.8 wt %, 1b forms a solution at pH 9.0 and 60 °C, and the solution remains after the conditions have been adjusted to pH 7.0 and room temperature. Further decreasing of the pH value of the solution of 1b to 4.0 results in an opaque hydrogel (Figure 1B), which lacks thermal reversibility and turns into white precipitates when it is heated to about 60 °C. Additionally, the white and opaque color of the hydrogel suggests that 1b tends to form microcrystals [65-68] that constitute the weakly cross-linked matrices of the hydrogel. The addition of a D-tyrosine phosphate residue to 1b affords the precursor 1e. Despite containing a D-tyrosine phosphate, 1e (0.8 wt %, pH 7.6) undergoes dephosphorylation in the presence of alkaline phosphatase (5.0 U/mL) to form the hydrogelator 1f, which results in a transparent hydrogel (Figure 1D). Unlike 1d, only 0.8 wt % of 1f is necessary to form the hydrogel at pH 7.6.
As a hydrogelator, 2a displays different characteristics to those of 2b. 2a (8.0 mg) dissolves in water (1.0 mL) at pH 9 when heated to 85 °C. The clear solution of 2a turns into a stable, thermally reversible, and slightly opaque hydrogel (Figure 1E) after being stored at room temperature for 12 h at pH 7.2. 2b exhibits a better solubility than 2a because 0.8 wt % of 2b gives a clear solution at pH 9.0 when being heating to 65 °C. Similarly, the solution of 2b turns into a semitransparent hydrogel (Figure 1F) after the pH is decreased to 7.2. 2b forms thermally reversible hydrogel within 2 min after its solution is cooled to room temperature from 65 °C, which is much faster than the hydrogelation of 2a. The commercially available flurbiprofen is the racemic mixture 3. Similar to the behavior of 2a, 3a (8.0 mg) dissolves in water (1.0 mL) at pH 9.0 and 75 °C, and the solution of 3a becomes a stable semitransparent hydrogel (Figure 1G) within 5 min at room temperature after the pH of the solution is adjusted to 7.2. Although being thermally reversible, the hydrogel of 3a exhibits poor recovery: the hydrogel of 3a takes more than 24 hours to recover from the sol–gel state after being disrupted by an external force. Being made from a racemic mixture of ibuprofen (4), 4a (8.0 mg) dissolves in water (1.0 mL) at pH 9 and 75 °C, and the solution of 4a becomes a stable semitransparent hydrogel (Figure 1H) after standing at room temperature and pH 7.2 overnight. Despite its thermal reversibility, 4a shows weak recovery properties. Compound 5a fails to form a hydrogel, likely due to the insufficient aromatic–aromatic interaction originating from the salicylic acid groups. In order to confirm that the aromatic–aromatic interactions originating from Phe–Phe are essential for the self-assembly of the hydrogelators of NSAIDs to form the nanofibers as the matrices of the hydrogels, we studied the gelation properties of the conjugates of NSAIDs and Ala–Ala, a nonaromatic dipeptide. The conjugates of NSAIDs and Ala–Ala, 1g, 3g, 4g, and 5g, behave differently from those conjugates that contain Phe–Phe. At a concentration of 0.8 wt %, while 1g and 3g afford white, opaque hydrogels at pH 4.0 and 1.0, respectively, compounds 4g and 5g fail to form a hydrogel. The hydrogels of 1g and 3g shrink within 30 min after hydrogelation and tend to precipitate at room temperature over 24 h, indicating poor stability of the hydrogels of 1g and 3g. This result further confirms the critical role of aromatic–aromatic interaction for stabilizing molecular self-assembly in water.
Transmission electron microscopy (TEM)
In addition to the macroscopic phase transition such as hydrogelation, another hallmark of molecular self-assembly in water is the formation of ordered nanostructures (e.g., nanofibers or nanoparticles). As revealed by the TEM images (Figure 2), the hydrogel of 1a comprises long nanofibers that entangle to form the network. The widths of nanofibers in the gel of 1a appear to be nonuniform, displaying minimum width at 6 nm and maximum width at 20 nm (Figure 2A). The TEM image of the hydrogel of 1b shows helical and rigid nanofibers with an average width of around 48 nm (Figure 2B), which is a different morphology from that of 1a, and likely contributes to the thermal irreversibility of the hydrogel of 1b. Besides, the low density of the network in hydrogel 1b (Figure S1, Supporting Information File 1) [64] agrees with its poor reversibility. As shown in Figure 2C and Figure 2D, both the hydrogels of 1d and 1f comprise uniform long nanofibers, whose average widths are 6–7 nm. The exceptional high density of nanofibers in the hydrogel of 1d likely originates from the relatively high concentration of 1d in the hydrogel.
![[1860-5397-9-104-2]](/bjoc/content/figures/1860-5397-9-104-2.jpg?scale=2.0&max-width=1024&background=FFFFFF)
Figure 2: The TEM images of the matrices of the hydrogels formed by (A) 1a (0.8 wt %, pH 7.0); (B) 1b (0.8 wt %, pH 4.0); (C) 1d (1.5 wt %, pH 7.6) formed by treating 1c with alkaline phosphatase (5.0 U/mL); (D) 1f (0.8 wt %, pH 7.6) formed by treating 1e with alkaline phosphatase (5.0 U/mL); (E) 2a (0.8 wt %, pH 7.2); (F) 2b (0.8 wt %, pH 7.2); (G) 3a (0.8 wt %, pH 7.2); (H) 4a (0.8 wt %, pH 7.2); (I) 1g (0.8 wt %, pH 4); (J) 3g (0.8 wt %, pH 1.0). The scale bar is 100 nm.
Figure 2: The TEM images of the matrices of the hydrogels formed by (A) 1a (0.8 wt %, pH 7.0); (B) 1b (0.8 wt...
The hydrogel of 2a comprises two kinds of nanostructures, i.e., nanofibers and nanoparticles, visible in the TEM images. As shown in Figure 2E, long nanofibers with an average width of 17 nm entangle together to form larger helical nanofibers with an average width of 30 nm. Higher-magnification TEM shows that the large helical fibers comprise fibrils of 17 nm in width (Figure S1, Supporting Information File 1) [64]. In addition to the presence of the nanofibers, the nanoparticles (10–20 nm in diameter) also exist in the hydrogel of 2a. Different from the hydrogel of 2a, hydrogel 2b comprises long, uniform nanofibers with an average width of 12 nm (Figure 2F). Interestingly, the TEM of the hydrogel of 3a presents similar nanostructures to those in the hydrogel of 2b. As shown in Figure 2G, the long uniform nanofibers in the hydrogel of 3a have an average width of 12 nm. Higher magnification of the TEM of the hydrogel of 3a indicates that the nanofibers of 3a consist of two nanofibrils with an average width of 6 nm (Figure S1, Supporting Information File 1) [64]. As shown in Figure 2H, the hydrogel of 4a also consists of uniform nanofibers with an average width of 13 nm. These nanofibers arrange into a network that has very low density. While the TEM image (Figure 2I) of the hydrogel of 1g clearly shows nanocrystals with a length over 450 nm and width varying from 35 nm to 200 nm, the TEM image (Figure 2J) of the hydrogel of 3g exhibits uniform nanotubes that have an outer width of 22 nm and inner width of 8 nm. These nanotubes form a poorly cross-linked network, which agrees with the instability of the hydrogel of 3g.
Rheology
Since viscoelasticity is an essential feature of hydrogels [69], we use rheometry to characterize the hydrogels. Based on the stability of these hydrogels, we choose to study the rheological properties of the hydrogels of 1a, 1b, 1d, 1f, 2a, 2b, 3a and 4a, and list their rheology data in Table 2. During the dynamic strain sweep, all these hydrogels, under constant oscillation frequencies and different oscillation strains, exhibit a strain-independent storage modulus (G') until reaching their critical strain, at which the values of G′ start to decrease drastically due to the breakdown of the networks of the hydrogels. In addition to the critical strain, the dynamic strain sweep provides the maximum G' values in the linear region. The naproxen-containing hydrogels show maximum storage moduli from 4.0 × 102 to 4.9 × 104 Pa (Table 2). The hydrogel of 1a has a maximum G' of 2.1 × 103 Pa and critical strain of 0.62%, and the hydrogel of 1b has the highest maximum G' (4.9 × 104 Pa), agreeing with the well cross-linked network in the hydrogel of 1b resulted from the long and wide (48 nm) nanofibers. Since the tyrosine residue renders 1d and 1f with better solubility than for 1a and 1b (Table S1, Supporting Information File 1) [64], the hydrogels of 1d and 1f have smaller maximum storage moduli (6.2 × 102 and 4.0 × 102 Pa) than do the hydrogels of 1a and 1b. The thin and flexible nanofibers in the hydrogels of 1d and 1f also agree with their rheological properties.
Table 2: The rheological properties and TEM characteristics of the NSAID-containing hydrogels.
| compound |
cgc
(wt %) |
max. G' a
(Pa) |
critical straina
(%) |
G' b
(Pa) |
nanofiber widthc
(nm) |
|---|---|---|---|---|---|
| 1a | 0.2 | 2100 | 0.62 | 1700 | 6–20 |
| 1b | 0.2 | 49000 | 1.0 | 53000 | 48 |
| 1dd | 1.0 | 620 | 0.39 | 610 | 6.5 |
| 1f | 0.2 | 400 | 1.6 | 620 | 7 |
| 2a | 0.2 | 150 | 0.96 | 150 | 17 |
| 2b | 0.2 | 890 | 1.8 | 990 | 12 |
| 3a | 0.2 | 1300 | 3.7 | 1500 | 6 |
| 4a | 0.3 | 7.8 | 0.57 | 13 | 13 |
aDynamic strain sweep; bDynamic frequency sweep, the value is taken at a frequency equal to 6.28 rad/s; cAverage; dThe concentration of hydrogel 1d is 1.5 wt %, while the others are 0.8 wt %.
(R)-Flurbiprofen-containing hydrogelators 2a and 2b exhibit maximum storage moduli of 1.5 × 102 and 8.7 × 102 Pa, respectively, which are smaller than those of the hydrogels of 1a and 1b. Such a difference is consistent with the less aromatic–aromatic interaction provided by the flurbiprofen motif due to its smaller conjugate system compared with the naproxen group in 1a and 1b. The maximum G' of the hydrogel of 2b (8.9 × 102 Pa) is larger than that of the hydrogel of 2a (1.5 × 102 Pa), agreeing with the higher density of the nanofibers in the hydrogel of 2b. Interestingly, the gel of 3a, which comprises 2a and (S)-flurbiprofen-FF, exhibits a higher maximum G' (1.3 × 103 Pa) in strain sweep and larger critical strain (3.7%) than those values of 2a or 2b, suggesting that the combination of 2a and (S)-flurbiprofen-FF affords a more stable hydrogel. This result agrees with the TEM image of 3a, which exhibits the highest density of its network among the flurbiprofen-containing hydrogels. Unlike the hydrogels containing naproxen or flurbiprofen, ibuprofen-containing hydrogel 4a behaves as a relatively weak hydrogel and exhibits a maximum G' of 7.8 Pa and critical strain 0.57%, clearly indicating that the isopropyl-substituted phenyl group is less efficient at providing aromatic–aromatic interaction for hydrogelation than naproxen or flubiprofen group are.
After obtaining the critical strains of the hydrogels, we measure the frequency dependence of their storage and loss moduli using dynamic frequency sweep at constant oscillation amplitude and temperature but varying oscillation frequency (0.1–200 rad/s). All of these hydrogels exhibit little dependence on frequency (Figure S3, Supporting Information File 1) [64], suggesting that the matrices of gels have good tolerance to the external shear force. In addition, the storage moduli of all these hydrogels in the frequency sweep are comparable with storage moduli of the constant region in the strain sweep. Hydrogel 1b has the highest G' (5.3 × 104 Pa), while hydrogels 1d and 1f appear to have the lowest two G' values (6.1 × 102 Pa and 6.2 × 102 Pa) among the naproxen-containing hydrogels. Hydrogels of 2a and 2b have smaller G' values, 1.5 × 102 Pa and 9.9 × 102 Pa, respectively, than those of hydrogels 1a and 1b, which likely originate from their structure difference. Hydrogel 3a has a G' value of 1.5 × 103 Pa, which is larger than that of hydrogel of 4a (13 Pa), partially due to more effective aromatic–aromatic interaction of the flurbiprofen groups compared to the ibuprofen.
Both hydrogels of 1a and 1d possess excellent thermal recovery properties (Figure S4, Supporting Information File 1) [64], indicating that these molecules self-assemble to re-establish the network rapidly after deformation caused by a perturbation. To characterize the recovery properties of the gels of 1a and 1d, we first measure the G' values of the gels at 0.4% strain for 10 min to obtain their original storage moduli, and then apply a large-amplitude oscillation with 100% strain and 6.28 rad/s angular frequency to perturb the structure of the hydrogels for 10 min. After removing this large amplitude of oscillation, we immediately measure the storage moduli of the gels at 0.4% of strain, and then calculate their recovery percentages by dividing them by their original moduli. As shown in Figure 3, G' of hydrogel 1a decreases to 0.5% of its original storage modulus when being exposed to the large-amplitude oscillation (100% of strain). After the removal of the applied large oscillation, the G' value of hydrogel 1a immediately recovers by 50% and reaches 100% recovery in less than 5 min. Similarly, hydrogel 1d also exhibits a fairly fast recovery of G'. The application of the large oscillation for 10 min decreases the G' of hydrogel 1d to 2.5% of its original storage modulus. As soon as the external large oscillation is stopped, hydrogel 1d recovers by 25% and reaches 100% recovery after 20 min. These data suggest that hydrogels 1a and 1d, like other supramolecular gels [70,71], are able to re-establish networks rapidly after deformation.
![[1860-5397-9-104-3]](/bjoc/content/figures/1860-5397-9-104-3.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 3: Recovery of the storage moduli of the gels formed by 0.8 wt % of 1a at pH 7.0 and 1.5 wt % of 1d formed by using alkaline phosphatase (5.0 U/mL) to treat the solution of 1c at pH 7.6.
Figure 3: Recovery of the storage moduli of the gels formed by 0.8 wt % of 1a at pH 7.0 and 1.5 wt % of 1d fo...
Cytotoxicity
To evaluate the biocompatibility of these NSAID hydrogelators, we select 1a, 1c, and 1d to test their cytotoxicity by incubating them with HeLa cells for 72 h at 37 °C. As shown in Figure 4, 1a, 1c, and 1d exhibit IC50 values of 206 µM, 321 µM, and 294 µM, respectively. Among these three hydrogels, 1a lacks the tyrosine residue and is less soluble in water, thus exhibiting relatively low IC50. All of 1a, 1c and 1d, exhibit IC50 values larger than 200 µM, suggesting that they are relatively biocompatible.
![[1860-5397-9-104-4]](/bjoc/content/figures/1860-5397-9-104-4.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 4: The IC50 values of 1a, 1c and 1d incubated with HeLa cells after 72 h.
Figure 4: The IC50 values of 1a, 1c and 1d incubated with HeLa cells after 72 h.
Conclusion
In conclusion, we have systematically investigated a new type of supramolecular hydrogelator made of nonsteroidal anti-inflammatory drugs (NSAIDs). The direct conjugation of NSAIDs and small peptides (Phe–Phe) generates molecules that self-assemble in water to form hydrogels. The large difference in gelation properties by changing small peptides from Phe–Phe to Ala–Ala confirms the important role of the aromatic–aromatic interaction between diphenylalanine groups [24]. In addition, the molecular structures of NSAIDs also affect their gelation stability. As a useful member in NSAIDs, naproxen conjugates with Phe–Phe to give a promising hydrogelator (NpxFF) that may act as a general motif to enable hydrogelation of other bioactive molecules. By providing useful insight for design of the NSAID hydrogelators, this approach contributes to the development of bioactive molecules that have dual or multiple roles, such as hydrogelators and therapeutic agents.
Supporting Information
| Supporting Information File 1: Experimental details. | ||
| Format: PDF | Size: 1.1 MB | Download |
References
-
Lee, K. Y.; Mooney, D. J. Chem. Rev. 2001, 101, 1869. doi:10.1021/cr000108x
Return to citation in text: [1] -
Karp, J. M.; Langer, R. Curr. Opin. Biotechnol. 2007, 18, 454. doi:10.1016/j.copbio.2007.09.008
Return to citation in text: [1] -
Lutolf, M. P.; Hubbell, J. A. Nat. Biotechnol. 2005, 23, 47. doi:10.1038/nbt1055
Return to citation in text: [1] -
Takashima, Y.; Yuting, Y.; Otsubo, M.; Yamaguchi, H.; Harada, A. Beilstein J. Org. Chem. 2012, 8, 1594. doi:10.3762/bjoc.8.182
Return to citation in text: [1] -
Drury, J. L.; Mooney, D. J. Biomaterials 2003, 24, 4337. doi:10.1016/S0142-9612(03)00340-5
Return to citation in text: [1] -
Uhrich, K. E.; Cannizzaro, S. M.; Langer, R. S.; Shakesheff, K. M. Chem. Rev. 1999, 99, 3181. doi:10.1021/cr940351u
Return to citation in text: [1] -
Peppas, N. A.; Hilt, J. Z.; Khademhosseini, A.; Langer, R. Adv. Mater. 2006, 18, 1345. doi:10.1002/adma.200501612
Return to citation in text: [1] -
Torchilin, V. P. J. Controlled Release 2001, 73, 137. doi:10.1016/S0168-3659(01)00299-1
Return to citation in text: [1] -
Brazel, C. S.; Peppas, N. A. Polymer 1999, 40, 3383. doi:10.1016/S0032-3861(98)00546-1
Return to citation in text: [1] -
Estroff, L. A.; Hamilton, A. D. Chem. Rev. 2004, 104, 1201. doi:10.1021/cr0302049
Return to citation in text: [1] -
Banerjee, S.; Das, R. K.; Maitra, U. J. Mater. Chem. 2009, 19, 6649. doi:10.1039/b819218a
Return to citation in text: [1] -
Adhikari, B.; Palui, G.; Banerjee, A. Soft Matter 2009, 5, 3452. doi:10.1039/b905985g
Return to citation in text: [1] -
Adams, D. J.; Topham, P. D. Soft Matter 2010, 6, 3707. doi:10.1039/c000813c
Return to citation in text: [1] -
Chen, J.; McNeil, A. J. J. Am. Chem. Soc. 2008, 130, 16496. doi:10.1021/ja807651a
Return to citation in text: [1] -
Dastidar, P. Chem. Soc. Rev. 2008, 37, 2699. doi:10.1039/b807346e
Return to citation in text: [1] -
King, K. N.; McNeil, A. J. Chem. Commun. 2010, 46, 3511. doi:10.1039/c002081h
Return to citation in text: [1] -
Qiu, Z.; Yu, H.; Li, J.; Wang, Y.; Zhang, Y. Chem. Commun. 2009, 3342. doi:10.1039/b822840j
Return to citation in text: [1] -
Hirst, A. R.; Coates, I. A.; Boucheteau, T. R.; Miravet, J. F.; Escuder, B.; Castelletto, V.; Hamley, I. W.; Smith, D. K. J. Am. Chem. Soc. 2008, 130, 9113. doi:10.1021/ja801804c
Return to citation in text: [1] -
Kameta, N.; Yoshida, K.; Masuda, M.; Shimizu, T. Chem. Mater. 2009, 21, 5892. doi:10.1021/cm903108h
Return to citation in text: [1] -
Liao, S. W.; Yu, T.-B.; Guan, Z. J. Am. Chem. Soc. 2009, 131, 17638. doi:10.1021/ja907097t
Return to citation in text: [1] -
Williams, R. J.; Smith, A. M.; Collins, R.; Hodson, N.; Das, A. K.; Ulijn, R. V. Nat. Nanotechnol. 2009, 4, 19. doi:10.1038/nnano.2008.378
Return to citation in text: [1] -
Wu, Z. L.; Kurokawa, T.; Liang, S.; Furukawa, H.; Gong, J. P. J. Am. Chem. Soc. 2010, 132, 10064. doi:10.1021/ja101969k
Return to citation in text: [1] -
Yang, Z.; Liang, G.; Xu, B. Acc. Chem. Res. 2008, 41, 315. doi:10.1021/ar7001914
Return to citation in text: [1] [2] -
Zhang, Y.; Kuang, Y.; Gao, Y.; Xu, B. Langmuir 2011, 27, 529. doi:10.1021/la1020324
Return to citation in text: [1] [2] -
Leong, W. L.; Tam, A. Y.-Y.; Batabyal, S. K.; Koh, L. W.; Kasapis, S.; Yam, V. W.-W.; Vittal, J. J. Chem. Commun. 2008, 3628. doi:10.1039/b807478j
Return to citation in text: [1] -
Schneider, J. P.; Pochan, D. J.; Ozbas, B.; Rajagopal, K.; Pakstis, L.; Kretsinger, J. J. Am. Chem. Soc. 2002, 124, 15030. doi:10.1021/ja027993g
Return to citation in text: [1] -
Collier, J. H.; Segura, T. Biomaterials 2011, 32, 4198. doi:10.1016/j.biomaterials.2011.02.030
Return to citation in text: [1] -
Lovell, J. F.; Roxin, A.; Ng, K. K.; Qi, Q.; McMullen, J. D.; DaCosta, R. S.; Zheng, G. Biomacromolecules 2011, 12, 3115. doi:10.1021/bm200784s
Return to citation in text: [1] -
Kumar, K. K.; Elango, M.; Subramanian, V.; Das, T. M. New J. Chem. 2009, 33, 1570. doi:10.1039/b821126d
Return to citation in text: [1] -
Zhang, S.; Holmes, T.; Lockshin, C.; Rich, A. Proc. Natl. Acad. Sci. U. S. A. 1993, 90, 3334. doi:10.1073/pnas.90.8.3334
Return to citation in text: [1] -
Silva, G. A.; Czeisler, C.; Niece, K. L.; Beniash, E.; Harrington, D. A.; Kessler, J. A.; Stupp, S. I. Science 2004, 303, 1352. doi:10.1126/science.1093783
Return to citation in text: [1] -
Jayawarna, V.; Ali, M.; Jowitt, T. A.; Miller, A. F.; Saiani, A.; Gough, J. E.; Ulijn, R. V. Adv. Mater. 2006, 18, 611. doi:10.1002/adma.200501522
Return to citation in text: [1] -
Yang, Z.; Ho, P.-L.; Liang, G.; Chow, K. H.; Wang, Q.; Cao, Y.; Guo, Z.; Xu, B. J. Am. Chem. Soc. 2007, 129, 266. doi:10.1021/ja0675604
Return to citation in text: [1] -
Xing, B.; Yu, C.-W.; Chow, K.-H.; Ho, P.-L.; Fu, D.; Xu, B. J. Am. Chem. Soc. 2002, 124, 14846. doi:10.1021/ja028539f
Return to citation in text: [1] -
Salick, D. A.; Kretsinger, J. K.; Pochan, D. J.; Schneider, J. P. J. Am. Chem. Soc. 2007, 129, 14793. doi:10.1021/ja076300z
Return to citation in text: [1] -
Yang, Z.; Liang, G.; Guo, Z.; Guo, Z.; Xu, B. Angew. Chem., Int. Ed. 2007, 46, 8216. doi:10.1002/anie.200701697
Return to citation in text: [1] -
Zhao, F.; Ma, M. L.; Xu, B. Chem. Soc. Rev. 2009, 38, 883. doi:10.1039/b806410p
Return to citation in text: [1] -
Brahmachari, S.; Debnath, S.; Dutta, S.; Das, P. K. Beilstein J. Org. Chem. 2010, 6, 859. doi:10.3762/bjoc.6.101
Return to citation in text: [1] -
Yang, Z. M.; Xu, B. Chem. Commun. 2004, 2424. doi:10.1039/b408897b
Return to citation in text: [1] -
Wang, Q.; Yang, Z.; Zhang, X.; Xiao, X.; Chang, C. K.; Xu, B. Angew. Chem., Int. Ed. 2007, 46, 4285. doi:10.1002/anie.200700404
Return to citation in text: [1] -
Gao, Y.; Kuang, Y.; Guo, Z.-F.; Guo, Z.; Krauss, I. J.; Xu, B. J. Am. Chem. Soc. 2009, 131, 13576. doi:10.1021/ja904411z
Return to citation in text: [1] -
Bouhadir, K. H.; Alsberg, E.; Mooney, D. J. Biomaterials 2001, 22, 2625. doi:10.1016/S0142-9612(01)00003-5
Return to citation in text: [1] -
Standley, S. M.; Toft, D. J.; Cheng, H.; Soukasene, S.; Chen, J.; Raja, S. M.; Band, V.; Band, H.; Cryns, V. L.; Stupp, S. I. Cancer Res. 2010, 70, 3020. doi:10.1158/0008-5472.CAN-09-3267
Return to citation in text: [1] -
Yang, Z. M.; Xu, K. M.; Guo, Z. F.; Guo, Z. H.; Xu, B. Adv. Mater. 2007, 19, 3152. doi:10.1002/adma.200701971
Return to citation in text: [1] -
Shi, J.; Gao, Y.; Yang, Z.; Xu, B. Beilstein J. Org. Chem. 2011, 7, 167. doi:10.3762/bjoc.7.23
Return to citation in text: [1] -
Pasc, A.; Akong, F. O.; Cosgun, S.; Gérardin, C. Beilstein J. Org. Chem. 2010, 6, 973. doi:10.3762/bjoc.6.109
Return to citation in text: [1] -
Vemula, P. K.; Li, J.; John, G. J. Am. Chem. Soc. 2006, 128, 8932. doi:10.1021/ja062650u
Return to citation in text: [1] -
Bhuniya, S.; Seo, Y. J.; Kim, B. H. Tetrahedron Lett. 2006, 47, 7153. doi:10.1016/j.tetlet.2006.08.002
Return to citation in text: [1] [2] -
Moore, R. A.; Tramèr, M. R.; Carroll, D.; Wiffen, P. J.; McQuay, H. J. BMJ 1998, 316, 333. doi:10.1136/bmj.316.7128.333
Return to citation in text: [1] -
Cevc, G.; Mazgareanu, S.; Rother, M.; Vierl, U. Int. J. Pharm. 2008, 359, 190. doi:10.1016/j.ijpharm.2008.04.005
Return to citation in text: [1] -
Lorenzo-Lamosa, M. L.; Remuñán-López, C.; Vila-Jato, J. L.; Alonso, M. J. J. Controlled Release 1998, 52, 109. doi:10.1016/S0168-3659(97)00203-4
Return to citation in text: [1] -
Csoka, G.; Racz, I.; Marton, S.; Balogh, E.; Farkas, E. Pharm. Ind. 1999, 61, 88.
Return to citation in text: [1] -
Banning, M. Expert Opin. Pharmacother. 2008, 9, 2921. doi:10.1517/14656566.9.16.2921
Return to citation in text: [1] -
Park, S. M.; Lee, Y. S.; Kim, B. H. Chem. Commun. 2003, 2912. doi:10.1039/b311249g
Return to citation in text: [1] -
Foster, J. A.; Piepenbrock, M.-O. M.; Lloyd, G. O.; Clarke, N.; Howard, J. A. K.; Steed, J. W. Nat. Chem. 2010, 2, 1037. doi:10.1038/nchem.859
Return to citation in text: [1] -
Bhuniya, S.; Park, S. M.; Kim, B. H. Org. Lett. 2005, 7, 1741. doi:10.1021/ol050300r
Return to citation in text: [1] -
Görbitz, C. H. Chem.–Eur. J. 2001, 7, 5153. doi:10.1002/1521-3765(20011203)7:23<5153::AID-CHEM5153>3.0.CO;2-N
Return to citation in text: [1] -
Li, J.; Kuang, Y.; Gao, Y.; Du, X.; Shi, J.; Xu, B. J. Am. Chem. Soc. 2013, 135, 542. doi:10.1021/ja310019x
Return to citation in text: [1] -
Branco, M. C.; Schneider, J. P. Acta Biomater. 2009, 5, 817. doi:10.1016/j.actbio.2008.09.018
Return to citation in text: [1] -
Hirano, Y.; Mooney, D. J. Adv. Mater. 2004, 16, 17. doi:10.1002/adma.200300383
Return to citation in text: [1] -
Vemula, P. K.; Cruikshank, G. A.; Karp, J. M.; John, G. Biomaterials 2009, 30, 383. doi:10.1016/j.biomaterials.2008.09.045
Return to citation in text: [1] -
Peer, D.; Karp, J. M.; Hong, S.; Farokhzad, O. C.; Margalit, R.; Langer, R. Nat. Nanotechnol. 2007, 2, 751. doi:10.1038/nnano.2007.387
Return to citation in text: [1] -
Liang, G.; Yang, Z.; Zhang, R.; Li, L.; Fan, Y.; Kuang, Y.; Gao, Y.; Wang, T.; Lu, W. W.; Xu, B. Langmuir 2009, 25, 8419. doi:10.1021/la804271d
Return to citation in text: [1] -
Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764
Return to citation in text: [1] [2] [3] [4] [5] [6] [7] -
Terech, P.; Weiss, R. G. Chem. Rev. 1997, 97, 3133. doi:10.1021/cr9700282
Return to citation in text: [1] -
Kar, T.; Debnath, S.; Das, D.; Shome, A.; Das, P. K. Langmuir 2009, 25, 8639. doi:10.1021/la804235e
Return to citation in text: [1] -
George, M.; Funkhouser, G. P.; Weiss, R. G. Langmuir 2008, 24, 3537. doi:10.1021/la703556d
Return to citation in text: [1] -
Ostuni, E.; Kamaras, P.; Weiss, R. G. Angew. Chem., Int. Ed. Engl. 1996, 35, 1324. doi:10.1002/anie.199613241
Return to citation in text: [1] -
Yan, C.; Pochan, D. J. Chem. Soc. Rev. 2010, 39, 3528. doi:10.1039/b919449p
Return to citation in text: [1] -
Adams, D. J.; Mullen, L. M.; Berta, M.; Chen, L.; Frith, W. J. Soft Matter 2010, 6, 1971. doi:10.1039/b921863g
Return to citation in text: [1] -
Mukhopadhyay, S.; Maitra, U.; Ira, K.; Krishnamoorthy, G.; Schmidt, J.; Talmon, Y. J. Am. Chem. Soc. 2004, 126, 15905. doi:10.1021/ja046788t
Return to citation in text: [1]
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 1. | Lee, K. Y.; Mooney, D. J. Chem. Rev. 2001, 101, 1869. doi:10.1021/cr000108x |
| 2. | Karp, J. M.; Langer, R. Curr. Opin. Biotechnol. 2007, 18, 454. doi:10.1016/j.copbio.2007.09.008 |
| 3. | Lutolf, M. P.; Hubbell, J. A. Nat. Biotechnol. 2005, 23, 47. doi:10.1038/nbt1055 |
| 4. | Takashima, Y.; Yuting, Y.; Otsubo, M.; Yamaguchi, H.; Harada, A. Beilstein J. Org. Chem. 2012, 8, 1594. doi:10.3762/bjoc.8.182 |
| 10. | Estroff, L. A.; Hamilton, A. D. Chem. Rev. 2004, 104, 1201. doi:10.1021/cr0302049 |
| 11. | Banerjee, S.; Das, R. K.; Maitra, U. J. Mater. Chem. 2009, 19, 6649. doi:10.1039/b819218a |
| 12. | Adhikari, B.; Palui, G.; Banerjee, A. Soft Matter 2009, 5, 3452. doi:10.1039/b905985g |
| 13. | Adams, D. J.; Topham, P. D. Soft Matter 2010, 6, 3707. doi:10.1039/c000813c |
| 14. | Chen, J.; McNeil, A. J. J. Am. Chem. Soc. 2008, 130, 16496. doi:10.1021/ja807651a |
| 15. | Dastidar, P. Chem. Soc. Rev. 2008, 37, 2699. doi:10.1039/b807346e |
| 16. | King, K. N.; McNeil, A. J. Chem. Commun. 2010, 46, 3511. doi:10.1039/c002081h |
| 17. | Qiu, Z.; Yu, H.; Li, J.; Wang, Y.; Zhang, Y. Chem. Commun. 2009, 3342. doi:10.1039/b822840j |
| 18. | Hirst, A. R.; Coates, I. A.; Boucheteau, T. R.; Miravet, J. F.; Escuder, B.; Castelletto, V.; Hamley, I. W.; Smith, D. K. J. Am. Chem. Soc. 2008, 130, 9113. doi:10.1021/ja801804c |
| 19. | Kameta, N.; Yoshida, K.; Masuda, M.; Shimizu, T. Chem. Mater. 2009, 21, 5892. doi:10.1021/cm903108h |
| 20. | Liao, S. W.; Yu, T.-B.; Guan, Z. J. Am. Chem. Soc. 2009, 131, 17638. doi:10.1021/ja907097t |
| 21. | Williams, R. J.; Smith, A. M.; Collins, R.; Hodson, N.; Das, A. K.; Ulijn, R. V. Nat. Nanotechnol. 2009, 4, 19. doi:10.1038/nnano.2008.378 |
| 22. | Wu, Z. L.; Kurokawa, T.; Liang, S.; Furukawa, H.; Gong, J. P. J. Am. Chem. Soc. 2010, 132, 10064. doi:10.1021/ja101969k |
| 23. | Yang, Z.; Liang, G.; Xu, B. Acc. Chem. Res. 2008, 41, 315. doi:10.1021/ar7001914 |
| 24. | Zhang, Y.; Kuang, Y.; Gao, Y.; Xu, B. Langmuir 2011, 27, 529. doi:10.1021/la1020324 |
| 25. | Leong, W. L.; Tam, A. Y.-Y.; Batabyal, S. K.; Koh, L. W.; Kasapis, S.; Yam, V. W.-W.; Vittal, J. J. Chem. Commun. 2008, 3628. doi:10.1039/b807478j |
| 45. | Shi, J.; Gao, Y.; Yang, Z.; Xu, B. Beilstein J. Org. Chem. 2011, 7, 167. doi:10.3762/bjoc.7.23 |
| 46. | Pasc, A.; Akong, F. O.; Cosgun, S.; Gérardin, C. Beilstein J. Org. Chem. 2010, 6, 973. doi:10.3762/bjoc.6.109 |
| 8. | Torchilin, V. P. J. Controlled Release 2001, 73, 137. doi:10.1016/S0168-3659(01)00299-1 |
| 9. | Brazel, C. S.; Peppas, N. A. Polymer 1999, 40, 3383. doi:10.1016/S0032-3861(98)00546-1 |
| 47. | Vemula, P. K.; Li, J.; John, G. J. Am. Chem. Soc. 2006, 128, 8932. doi:10.1021/ja062650u |
| 48. | Bhuniya, S.; Seo, Y. J.; Kim, B. H. Tetrahedron Lett. 2006, 47, 7153. doi:10.1016/j.tetlet.2006.08.002 |
| 7. | Peppas, N. A.; Hilt, J. Z.; Khademhosseini, A.; Langer, R. Adv. Mater. 2006, 18, 1345. doi:10.1002/adma.200501612 |
| 40. | Wang, Q.; Yang, Z.; Zhang, X.; Xiao, X.; Chang, C. K.; Xu, B. Angew. Chem., Int. Ed. 2007, 46, 4285. doi:10.1002/anie.200700404 |
| 70. | Adams, D. J.; Mullen, L. M.; Berta, M.; Chen, L.; Frith, W. J. Soft Matter 2010, 6, 1971. doi:10.1039/b921863g |
| 71. | Mukhopadhyay, S.; Maitra, U.; Ira, K.; Krishnamoorthy, G.; Schmidt, J.; Talmon, Y. J. Am. Chem. Soc. 2004, 126, 15905. doi:10.1021/ja046788t |
| 5. | Drury, J. L.; Mooney, D. J. Biomaterials 2003, 24, 4337. doi:10.1016/S0142-9612(03)00340-5 |
| 6. | Uhrich, K. E.; Cannizzaro, S. M.; Langer, R. S.; Shakesheff, K. M. Chem. Rev. 1999, 99, 3181. doi:10.1021/cr940351u |
| 41. | Gao, Y.; Kuang, Y.; Guo, Z.-F.; Guo, Z.; Krauss, I. J.; Xu, B. J. Am. Chem. Soc. 2009, 131, 13576. doi:10.1021/ja904411z |
| 42. | Bouhadir, K. H.; Alsberg, E.; Mooney, D. J. Biomaterials 2001, 22, 2625. doi:10.1016/S0142-9612(01)00003-5 |
| 43. | Standley, S. M.; Toft, D. J.; Cheng, H.; Soukasene, S.; Chen, J.; Raja, S. M.; Band, V.; Band, H.; Cryns, V. L.; Stupp, S. I. Cancer Res. 2010, 70, 3020. doi:10.1158/0008-5472.CAN-09-3267 |
| 44. | Yang, Z. M.; Xu, K. M.; Guo, Z. F.; Guo, Z. H.; Xu, B. Adv. Mater. 2007, 19, 3152. doi:10.1002/adma.200701971 |
| 24. | Zhang, Y.; Kuang, Y.; Gao, Y.; Xu, B. Langmuir 2011, 27, 529. doi:10.1021/la1020324 |
| 32. | Jayawarna, V.; Ali, M.; Jowitt, T. A.; Miller, A. F.; Saiani, A.; Gough, J. E.; Ulijn, R. V. Adv. Mater. 2006, 18, 611. doi:10.1002/adma.200501522 |
| 34. | Xing, B.; Yu, C.-W.; Chow, K.-H.; Ho, P.-L.; Fu, D.; Xu, B. J. Am. Chem. Soc. 2002, 124, 14846. doi:10.1021/ja028539f |
| 35. | Salick, D. A.; Kretsinger, J. K.; Pochan, D. J.; Schneider, J. P. J. Am. Chem. Soc. 2007, 129, 14793. doi:10.1021/ja076300z |
| 36. | Yang, Z.; Liang, G.; Guo, Z.; Guo, Z.; Xu, B. Angew. Chem., Int. Ed. 2007, 46, 8216. doi:10.1002/anie.200701697 |
| 37. | Zhao, F.; Ma, M. L.; Xu, B. Chem. Soc. Rev. 2009, 38, 883. doi:10.1039/b806410p |
| 38. | Brahmachari, S.; Debnath, S.; Dutta, S.; Das, P. K. Beilstein J. Org. Chem. 2010, 6, 859. doi:10.3762/bjoc.6.101 |
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 31. | Silva, G. A.; Czeisler, C.; Niece, K. L.; Beniash, E.; Harrington, D. A.; Kessler, J. A.; Stupp, S. I. Science 2004, 303, 1352. doi:10.1126/science.1093783 |
| 23. | Yang, Z.; Liang, G.; Xu, B. Acc. Chem. Res. 2008, 41, 315. doi:10.1021/ar7001914 |
| 39. | Yang, Z. M.; Xu, B. Chem. Commun. 2004, 2424. doi:10.1039/b408897b |
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 30. | Zhang, S.; Holmes, T.; Lockshin, C.; Rich, A. Proc. Natl. Acad. Sci. U. S. A. 1993, 90, 3334. doi:10.1073/pnas.90.8.3334 |
| 26. | Schneider, J. P.; Pochan, D. J.; Ozbas, B.; Rajagopal, K.; Pakstis, L.; Kretsinger, J. J. Am. Chem. Soc. 2002, 124, 15030. doi:10.1021/ja027993g |
| 27. | Collier, J. H.; Segura, T. Biomaterials 2011, 32, 4198. doi:10.1016/j.biomaterials.2011.02.030 |
| 28. | Lovell, J. F.; Roxin, A.; Ng, K. K.; Qi, Q.; McMullen, J. D.; DaCosta, R. S.; Zheng, G. Biomacromolecules 2011, 12, 3115. doi:10.1021/bm200784s |
| 29. | Kumar, K. K.; Elango, M.; Subramanian, V.; Das, T. M. New J. Chem. 2009, 33, 1570. doi:10.1039/b821126d |
| 33. | Yang, Z.; Ho, P.-L.; Liang, G.; Chow, K. H.; Wang, Q.; Cao, Y.; Guo, Z.; Xu, B. J. Am. Chem. Soc. 2007, 129, 266. doi:10.1021/ja0675604 |
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 53. | Banning, M. Expert Opin. Pharmacother. 2008, 9, 2921. doi:10.1517/14656566.9.16.2921 |
| 49. | Moore, R. A.; Tramèr, M. R.; Carroll, D.; Wiffen, P. J.; McQuay, H. J. BMJ 1998, 316, 333. doi:10.1136/bmj.316.7128.333 |
| 50. | Cevc, G.; Mazgareanu, S.; Rother, M.; Vierl, U. Int. J. Pharm. 2008, 359, 190. doi:10.1016/j.ijpharm.2008.04.005 |
| 51. | Lorenzo-Lamosa, M. L.; Remuñán-López, C.; Vila-Jato, J. L.; Alonso, M. J. J. Controlled Release 1998, 52, 109. doi:10.1016/S0168-3659(97)00203-4 |
| 52. | Csoka, G.; Racz, I.; Marton, S.; Balogh, E.; Farkas, E. Pharm. Ind. 1999, 61, 88. |
| 64. | Ma, M.; Kuang, Y.; Gao, Y.; Zhang, Y.; Gao, P.; Xu, B. J. Am. Chem. Soc. 2010, 132, 2719. doi:10.1021/ja9088764 |
| 65. | Terech, P.; Weiss, R. G. Chem. Rev. 1997, 97, 3133. doi:10.1021/cr9700282 |
| 66. | Kar, T.; Debnath, S.; Das, D.; Shome, A.; Das, P. K. Langmuir 2009, 25, 8639. doi:10.1021/la804235e |
| 67. | George, M.; Funkhouser, G. P.; Weiss, R. G. Langmuir 2008, 24, 3537. doi:10.1021/la703556d |
| 68. | Ostuni, E.; Kamaras, P.; Weiss, R. G. Angew. Chem., Int. Ed. Engl. 1996, 35, 1324. doi:10.1002/anie.199613241 |
| 61. | Vemula, P. K.; Cruikshank, G. A.; Karp, J. M.; John, G. Biomaterials 2009, 30, 383. doi:10.1016/j.biomaterials.2008.09.045 |
| 62. | Peer, D.; Karp, J. M.; Hong, S.; Farokhzad, O. C.; Margalit, R.; Langer, R. Nat. Nanotechnol. 2007, 2, 751. doi:10.1038/nnano.2007.387 |
| 63. | Liang, G.; Yang, Z.; Zhang, R.; Li, L.; Fan, Y.; Kuang, Y.; Gao, Y.; Wang, T.; Lu, W. W.; Xu, B. Langmuir 2009, 25, 8419. doi:10.1021/la804271d |
| 58. | Li, J.; Kuang, Y.; Gao, Y.; Du, X.; Shi, J.; Xu, B. J. Am. Chem. Soc. 2013, 135, 542. doi:10.1021/ja310019x |
| 59. | Branco, M. C.; Schneider, J. P. Acta Biomater. 2009, 5, 817. doi:10.1016/j.actbio.2008.09.018 |
| 60. | Hirano, Y.; Mooney, D. J. Adv. Mater. 2004, 16, 17. doi:10.1002/adma.200300383 |
| 48. | Bhuniya, S.; Seo, Y. J.; Kim, B. H. Tetrahedron Lett. 2006, 47, 7153. doi:10.1016/j.tetlet.2006.08.002 |
| 54. | Park, S. M.; Lee, Y. S.; Kim, B. H. Chem. Commun. 2003, 2912. doi:10.1039/b311249g |
| 55. | Foster, J. A.; Piepenbrock, M.-O. M.; Lloyd, G. O.; Clarke, N.; Howard, J. A. K.; Steed, J. W. Nat. Chem. 2010, 2, 1037. doi:10.1038/nchem.859 |
| 56. | Bhuniya, S.; Park, S. M.; Kim, B. H. Org. Lett. 2005, 7, 1741. doi:10.1021/ol050300r |
| 57. | Görbitz, C. H. Chem.–Eur. J. 2001, 7, 5153. doi:10.1002/1521-3765(20011203)7:23<5153::AID-CHEM5153>3.0.CO;2-N |
© 2013 Li et al; licensee Beilstein-Institut.
This is an Open Access article under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The license is subject to the Beilstein Journal of Organic Chemistry terms and conditions: (http://www.beilstein-journals.org/bjoc)